polymyalgia rheumatica
- Related: Step 3, Allergy and Immunology, fibromyalgia vs polymyositis vs polymyalgia rheumatica
- tags: #rheumatology
Polymyalgia rheumatica is an autoimmune disease with several sites of muscle and joint pain and it is commonly associated with temporal arteritis.
Polymyalgia rheumatica is more common in:
- Women
- People of northern European descent (i.e., Scandinavian countries)
- The elderly (peak incidence between 70 and 80 years old)
Symptoms
The presentation of polymyalgia rheumatica includes symmetrical morning muscle stiffness and pain in the neck, shoulders, and hips. Morning stiffness lasting >1 hour.
Physical exam findings include fatigue, edema of the extremities, tenderness to palpation, movement limited by pain, but normal muscle strength unlike polymyositis, which presents with decreased muscle strength.
In PMR, the physical examination is frequently unremarkable with patients having no focal tenderness or pain with active or passive range of motion. Signs of inflammation in the joints are absent. When asked to identify the location of their pain, patients typically indicate the soft tissues and not the joints.
Diagnosis
Laboratory findings in polymyalgia rheumatica include decreased hematocrit with increased ESR.
MRI of polymyalgia rheumatica is associated with increased signal at tendon sheaths and tissue outside of joints.
Because polymyalgia rheumatica has such a strong correlation with temporal arteritis, patients should automatically be worked up for it as well.
Treatment
Treatment of polymyalgia rheumatica involves low dose corticosteroids that are slowly tapered.
Uworld
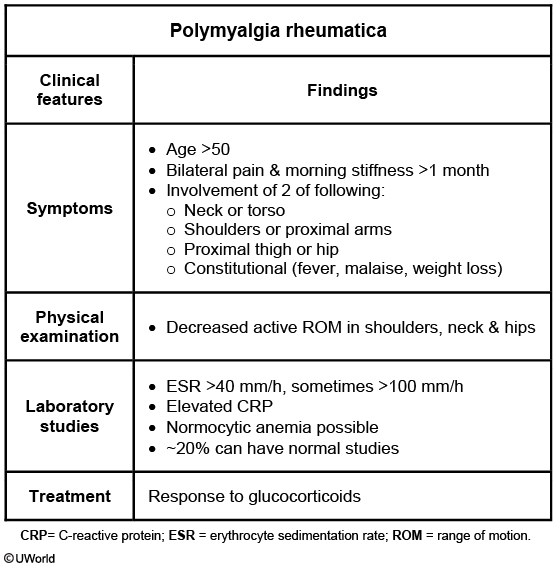
This patient with bilateral shoulder pain and stiffness most likely has polymyalgia rheumatica (PMR), a condition that occurs almost exclusively in individuals age >50. Patients characteristically have aching pain and stiffness that involve the shoulders, neck, and/or hip girdle and are often worse in the morning. Difficulty getting dressed is common, and malaise, fatigue, and weight loss are often reported. Muscle strength is typically intact, but range of motion may be decreased. Inflammatory markers (eg, erythrocyte sedimentation rate, C-reactive protein) are typically elevated on laboratory testing.
A minority of cases are associated with giant cell arteritis (GCA), a vasculitis characterized by localized headache, jaw claudication, and visual disturbances that can eventually result in blindness. In the absence of clinical findings suggestive of GCA, the treatment of PMR consists of low-dose glucocorticoids (eg, prednisone 20 mg daily), which provides rapid symptomatic relief of pain. In fact, the response to glucocorticoids is typically so complete that persistent symptoms should prompt consideration of alternative diagnoses.
Virtually 100% of patients with PMR respond rapidly to glucocorticoid treatment; however, symptoms may relapse in up to half after the steroid dosage is tapered.
Although both PMR and rheumatoid arthritis (RA) can cause aching pain and stiffness, only RA causes joint destruction. These diseases can be differentiated by the distribution of symptoms: PMR causes proximal symptoms (eg, shoulders, hip girdle), whereas RA tends to affect smaller, more distal joints (eg, metacarpophalangeal joints, proximal interphalangeal joints, wrists) and results in joint swelling and deformity.